Page 1
Loading page ...
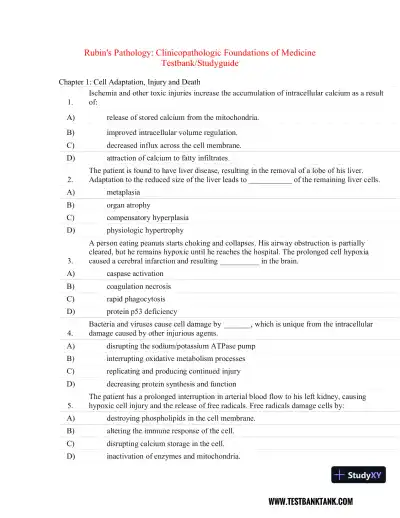
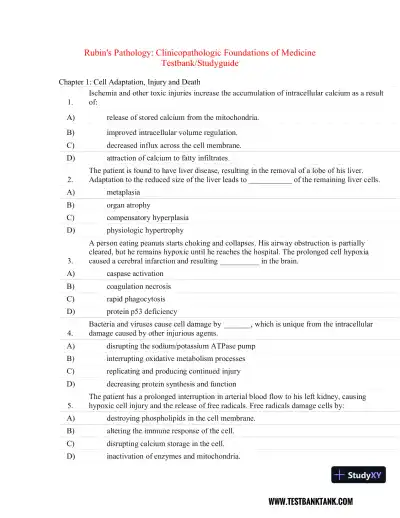
Sharpen your test-taking skills with Rubin's Pathology: Clinicopathologic Foundations of Medicine Seventh Edition Test Bank, designed for maximum learning.
Loading page ...
This document has 227 pages. Sign in to access the full document!