Page 1
Loading page ...
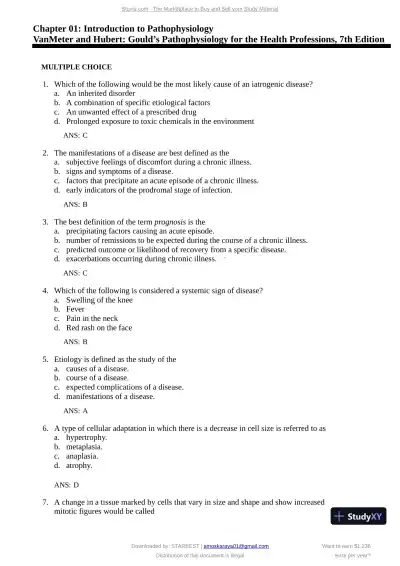
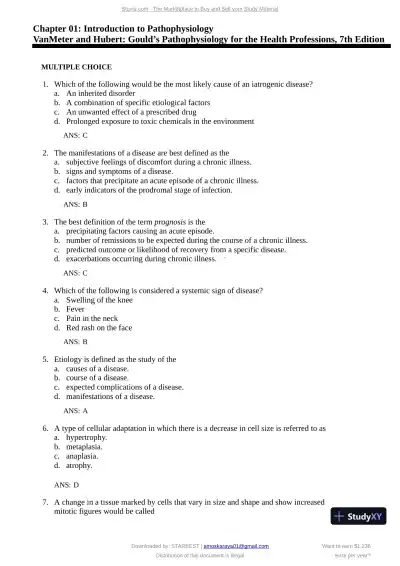
Sharpen your test-taking skills with Test Bank for Gould's Pathophysiology for the Health Professions, 7th Edition (Chapters 1-28), designed for maximum learning.
Loading page ...
This document has 219 pages. Sign in to access the full document!