Page 1
Loading page ...
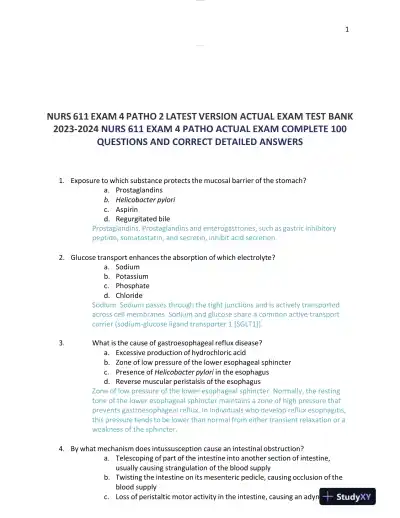
2023-2024 NURS611 Pathophysiology Exam 4 Version Test Bank With Answers provides real past exam questions to help you practice and improve your test-taking skills.
Loading page ...
This document has 27 pages. Sign in to access the full document!