Page 1
Loading page ...
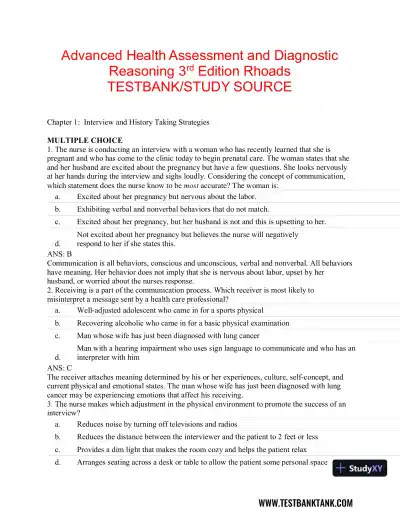
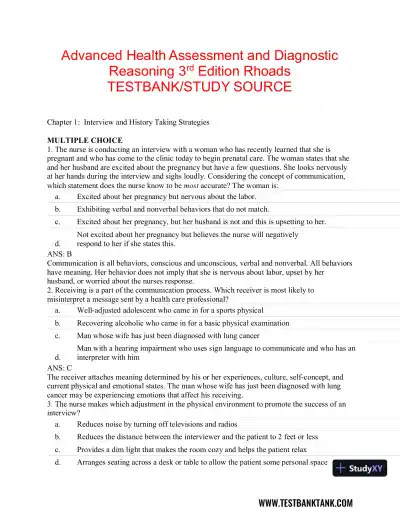
Get ahead in your studies with Advanced Health Assessment and Diagnostic Reasoning, 3rd Edition Test Bank, featuring exam-focused questions and solutions.
Loading page ...
This document has 206 pages. Sign in to access the full document!