Page 1
Loading page ...
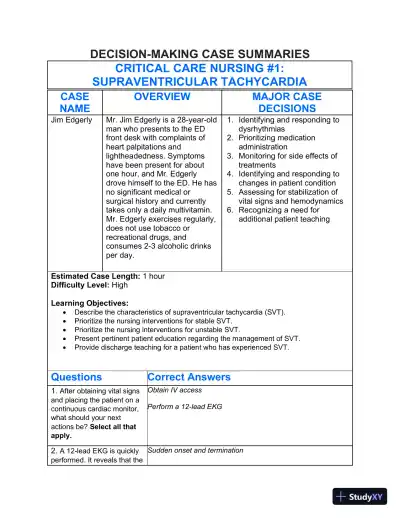
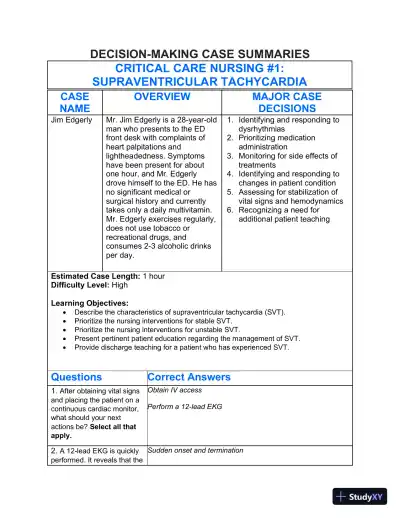
Solution Manual for Understanding the Essentials of Critical Care Nursing, 3rd Edition helps you reinforce learning with in-depth, accurate solutions.
Loading page ...
This document has 36 pages. Sign in to access the full document!